by Michael Bailey | Jan 28, 2020 | Environment & Ecology, Health & Medicine |
It may have started with a bat in a cave, but human activity set it loose.
By David Quammen, Via NYTimes
Jan. 28, 2020

A normally busy shopping district during the Chinese New Year holiday in Beijing.
The latest scary new virus that has captured the world’s horrified attention, caused a lockdown of 56 million people in China, disrupted travel plans around the globe and sparked a run on medical masks from Wuhan, Hubei Province, to Bryan, Texas, is known provisionally as “nCoV-2019.” It’s a clunky moniker for a lurid threat.
The name, picked by the team of Chinese scientists who isolated and identified the virus, is short for “novel coronavirus of 2019.” It reflects the fact that the virus was first recognized to have infected humans late last year — in a seafood and live-animal market in Wuhan — and that it belongs to the coronavirus family, a notorious group. The SARS epidemic of 2002-3, which infected 8,098 people worldwide, killing 774 of them, was caused by a coronavirus, and so was the MERS outbreak that began on the Arabian Peninsula in 2012 and still lingers (2,494 people infected and 858 deaths as of November).
Despite the new virus’s name, though, and as the people who christened it well know, nCoV-2019 isn’t as novel as you might think.
Something very much like it was found several years ago in a cave in Yunnan, a province roughly a thousand miles southwest of Wuhan, by a team of perspicacious researchers, who noted its existence with concern. The fast spread of nCoV-2019 — more than 4,500 confirmed cases, including at least 106 deaths, as of Tuesday morning, and the figures will have risen by the time you read this — is startling but not unforeseeable. That the virus emerged from a nonhuman animal, probably a bat, and possibly after passing through another creature, may seem spooky, yet it is utterly unsurprising to scientists who study these things.
One such scientist is Zheng-Li Shi, of the Wuhan Institute of Virology, a senior author of the draft paper (not yet peer reviewed and so far available only in preprint) that gave nCoV-2019 its identity and name. It was Ms. Shi and her collaborators who, back in 2005, showed that the SARS pathogen was a bat virus that had spilled over into people. Ms. Shi and colleagues have been tracing coronaviruses in bats since then, warning that some of them are uniquely suited to cause human pandemics.
In a 2017 paper, they set out how, after nearly five years of collecting fecal samples from bats in the Yunnan cave, they had found coronaviruses in multiple individuals of four different species of bats, including one called the intermediate horseshoe bat, because of the half-oval flap of skin protruding like a saucer around its nostrils. The genome of that virus, Ms. Shi and her colleagues have now announced, is 96 percent identical to the Wuhan virus that has recently been found in humans. And those two constitute a pair distinct from all other known coronaviruses, including the one that causes SARS. In this sense, nCoV-2019 is novel — and possibly even more dangerous to humans than the other coronaviruses.
I say “possibly” because so far, not only do we not know how dangerous it is, we can’t know. Outbreaks of new viral diseases are like the steel balls in a pinball machine: You can slap your flippers at them, rock the machine on its legs and bonk the balls to the jittery rings, but where they end up dropping depends on 11 levels of chance as well as on anything you do. This is true with coronaviruses in particular: They mutate often while they replicate, and can evolve as quickly as a nightmare ghoul.
Peter Daszak, the president of EcoHealth Alliance, a private research organization based in New York that focuses on the connections between human and wildlife health, is one of Ms. Shi’s longtime partners. “We’ve been raising the flag on these viruses for 15 years,” he told me on Friday with calm frustration. “Ever since SARS.” He was a co-author of the 2005 bats-and-SARS study, and again of the 2017 paper about the multiple SARS-like coronaviruses in the Yunnan cave.
Mr. Daszak told me that, during that second study, the field team took blood samples from a couple of thousand Yunnanese people, about 400 of whom lived near the cave. Roughly 3 percent of them carried antibodies against SARS-related coronaviruses.
“We don’t know if they got sick. We don’t know if they were exposed as children or adults,” Mr. Daszak said. “But what it tells you is that these viruses are making the jump, repeatedly, from bats to humans.” In other words, this Wuhan emergency is no novel event. It’s part of a sequence of related contingencies that stretches back into the past and will stretch forward into the future, as long as current circumstances persist.
So when you’re done worrying about this outbreak, worry about the next one. Or do something about the current circumstances.
Current circumstances include a perilous trade in wildlife for food, with supply chains stretching through Asia, Africa and to a lesser extent, the United States and elsewhere. That trade has now been outlawed in China, on a temporary basis; but it was outlawed also during SARS, then allowed to resume — with bats, civets, porcupines, turtles, bamboo rats, many kinds of birds and other animals piled together in markets such as the one in Wuhan.
Current circumstances also include 7.6 billion hungry humans: some of them impoverished and desperate for protein; some affluent and wasteful and empowered to travel every which way by airplane. These factors are unprecedented on planet Earth: We know from the fossil record, by absence of evidence, that no large-bodied animal has ever been nearly so abundant as humans are now, let alone so effective at arrogating resources. And one consequence of that abundance, that power, and the consequent ecological disturbances is increasing viral exchanges — first from animal to human, then from human to human, sometimes on a pandemic scale.
We invade tropical forests and other wild landscapes, which harbor so many species of animals and plants — and within those creatures, so many unknown viruses. We cut the trees; we kill the animals or cage them and send them to markets. We disrupt ecosystems, and we shake viruses loose from their natural hosts. When that happens, they need a new host. Often, we are it.
The list of such viruses emerging into humans sounds like a grim drumbeat: Machupo, Bolivia, 1961; Marburg, Germany, 1967; Ebola, Zaire and Sudan, 1976; H.I.V., recognized in New York and California, 1981; a form of Hanta (now known as Sin Nombre), southwestern United States, 1993; Hendra, Australia, 1994; bird flu, Hong Kong, 1997; Nipah, Malaysia, 1998; West Nile, New York, 1999; SARS, China, 2002-3; MERS, Saudi Arabia, 2012; Ebola again, West Africa, 2014. And that’s just a selection. Now we have nCoV-2019, the latest thump on the drum.
Current circumstances also include bureaucrats who lie and conceal bad news, and elected officials who brag to the crowd about cutting forests to create jobs in the timber industry and agriculture or about cutting budgets for public health and research. The distance from Wuhan or the Amazon to Paris, Toronto or Washington is short for some viruses, measured in hours, given how well they can ride within airplane passengers. And if you think funding pandemic preparedness is expensive, wait until you see the final cost of nCoV-2019.
Fortunately, current circumstances also include brilliant, dedicated scientists and outbreak-response medical people — such as many at the Wuhan Institute of Virology, EcoHealth Alliance, the United States Centers for Disease Control and Prevention (C.D.C.), the Chinese C.D.C. and numerous other institutions. These are the people who go into bat caves, swamps and high-security containment laboratories, often risking their lives, to bring out bat feces and blood and other precious evidence to study genomic sequences and answer the key questions.
As the number of nCoV-2019 cases has increased, and the death toll along with it, one metric, the case fatality rate, has remained rather steady so far: at about or below 3 percent. As of Tuesday, less than three out of 100 confirmed cases had died. That’s relatively good luck — worse than for most strains of influenza, better than for SARS.
This good luck may not last. Nobody knows where the pinball will go. Four days from today, the number of cases may be in the tens of thousands. Six months from today, Wuhan pneumonia may be receding into memory. Or not.
We are faced with two mortal challenges, in the short term and the long term. Short term: We must do everything we can, with intelligence, calm and a full commitment of resources, to contain and extinguish this nCoV-2019 outbreak before it becomes, as it could, a devastating global pandemic. Long term: We must remember, when the dust settles, that nCoV-2019 was not a novel event or a misfortune that befell us. It was — it is — part of a pattern of choices that we humans are making.
David Quammen is an author and journalist whose books include “Spillover: Animal Infections and the Next Human Pandemic.”

by Michael Bailey | May 29, 2019 | Health & Medicine |
How one molecule from the cannabis plant
came to be seen as a therapeutic cure-all.
Excellent coverage, and a must-read for anyone interested in this soon-to-be explosive market.
To access the full feature online, via NYTimes subscription, or complimentary access, please use the direct links below. Otherwise, the full article is pasted-in following the links.
Direct links to article:
https://www.nytimes.com/interactive/2019/05/14/magazine/cbd-cannabis-cure.html
Via NYTimes, By MOISES VELASQUEZ-MANOFF, MAY 14, 2019
When Catherine Jacobson first heard about the promise of cannabis, she was at wits’ end. Her 3-year-old son, Ben, had suffered from epileptic seizures since he was 3 months old, a result of a brain malformation called polymicrogyria. Over the years, Jacobson and her husband, Aaron, have tried giving him at least 16 different drugs, but none provided lasting relief. They lived with the grim prognosis that their son — whose cognitive abilities never advanced beyond those of a 1-year-old — would likely continue to endure seizures until the cumulative brain injuries led to his death.
In early 2012, when Jacobson learned about cannabis at a conference organized by the Epilepsy Therapy Project, she felt a flicker of hope. The meeting, in downtown San Francisco, was unlike others she had attended, which were usually geared toward lab scientists and not directly focused on helping patients. This gathering aimed to get new treatments into patients’ hands as quickly as possible. Attendees weren’t just scientists and people from the pharmaceutical industry. They also included, on one day of the event, families of patients with epilepsy.
The tip came from a father named Jason David, with whom Jacobson began talking by chance outside a presentation hall. He wasn’t a presenter or even very interested in the goings-on at the conference. He had mostly lost faith in conventional medicine during his own family’s ordeal. But he claimed to have successfully treated his son’s seizures with a cannabis extract, and now he was trying to spread the word to anyone who would listen.
The idea to try cannabis extract came to David after he found out that the federal government held a patent on cannabidiol, a molecule derived from the cannabis plant that is commonly referred to as CBD. Unlike the better-known marijuana molecule delta-9-tetrahydrocannabinol, or THC, CBD isn’t psychoactive; it doesn’t get users high. But in the late 1990s, scientists at the National Institutes of Health discovered that it could produce remarkable medicinal effects. In test tubes, the molecule shielded neurons from oxidative stress, a damaging process common in many neurological disorders, including epilepsy.
Jacobson had a Ph.D. in neuroscience. She had started her postdoctoral research at the University of California, San Francisco, by studying how cancer cells metastasize and spread, but after Ben was born, she moved to Stanford and switched her focus to epilepsy — a shift that compounded her anguish. She often wept in the parking lot before heading into the lab, overwhelmed by dread at the prospect of deliberately causing epilepsy in rodents. “I couldn’t watch animals seize all day and then watch Ben seize all night,” she told me. “It was just too much.”
After meeting David and reading through the small body of published work on CBD, Jacobson changed postdoctoral directions once again, from primary research to the study of this community of parents who were treating their epileptic children with cannabis extracts. In reality, she was preparing to join it herself. One small, double-blind study particularly caught her attention. In 1980, scientists in Brazil treated eight epileptic patients with CBD and eight patients with sugar pills as a placebo. For half the group that received CBD, the seizures almost completely disappeared; another three experienced a reduction in the intensity of their seizures. Only one person in the placebo group got better.
The epilepsy drugs that had been approved to date, none of which had helped Ben much, typically targeted the same few ion channels and receptors on the surface of neurons. But CBD worked on different and still somewhat mysterious pathways. If she could find a suitable CBD extract, Jacobson thought, she might have a truly new class of drug for Ben. The other experimental drugs and devices she had heard about at epilepsy conferences were under development, unapproved by the F.D.A. and thus largely unavailable. But medical marijuana had been legal in California since 1996, so CBD was theoretically accessible right away.
[Read more on why CBD is everywhere.]
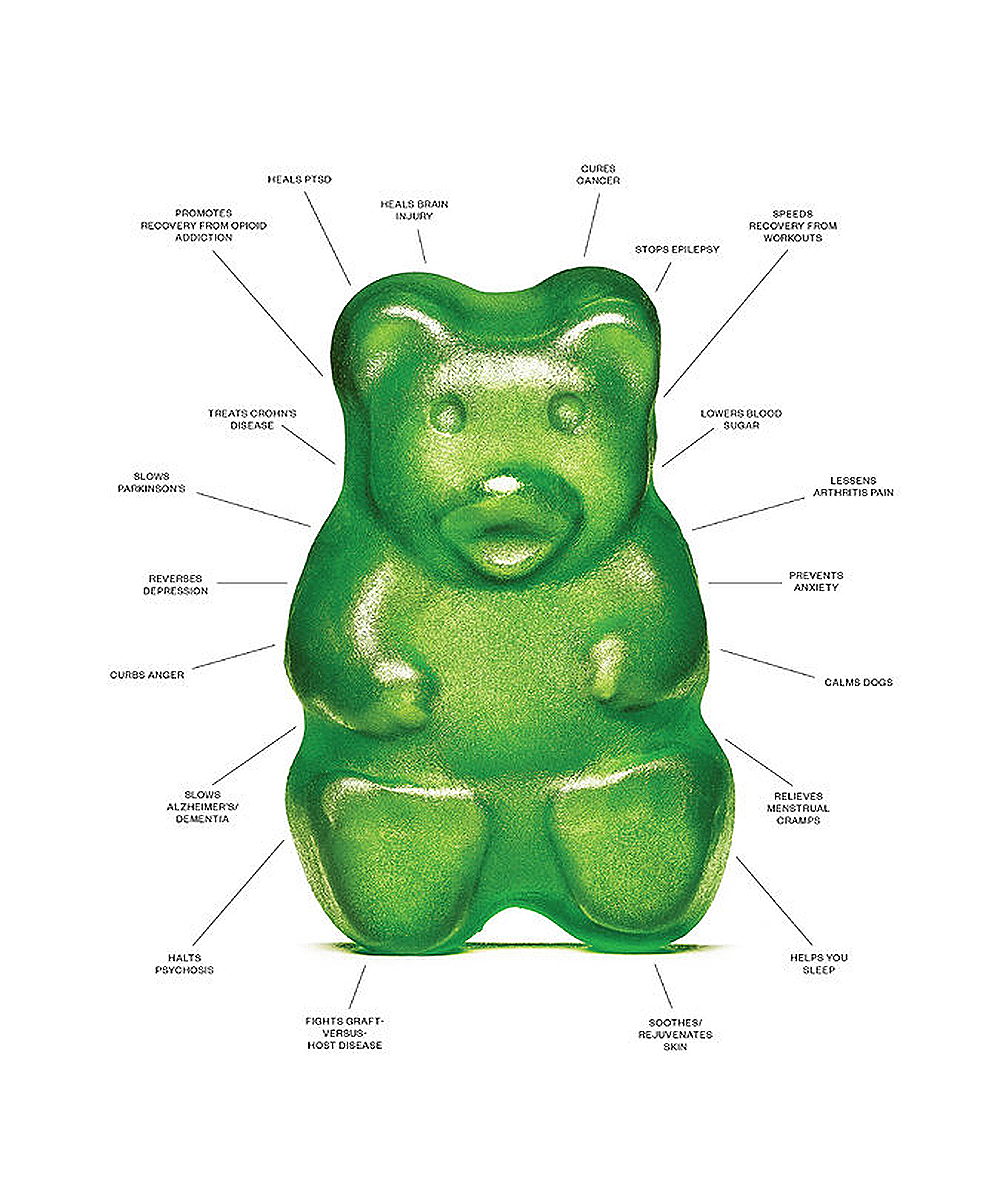
Seven years later, cannabidiol is everywhere. We are bombarded by a dizzying variety of CBD-infused products: beers, gummies, chocolates and marshmallows; lotions to rub on aching joints; oils to swallow; vaginal suppositories for “soothing,” in one company’s words, “the area that needs it most.” CVS and Walgreens each recently announced plans to sell CBD products in certain states. Jason David now sells a cannabis extract called Jayden’s Juice, named for his son — one of several extracts on the market, including Haleigh’s Hope and Charlotte’s Web, that are named after children who are said to have benefited from being treated with CBD.
Many of these products are vague about what exactly CBD can do. (The F.D.A. prohibits unproven health claims.) Yet promises abound on the internet, where numerous articles and testimonials suggest that CBD can effectively treat not just epilepsy but also anxiety, pain, sleeplessness, Crohn’s disease, arthritis and even anger. A confluence of factors has led to this strange moment. Plenty of legitimate, if still inconclusive, research is being done on CBD. Many scientists are truly excited about it. The laws governing cannabis and its chemical components have loosened up. And the anecdotes that have emerged from what Elizabeth Thiele, an epileptologist at Harvard, calls the “vernacular” cannabis movement have lent emotional force to the claims made for CBD.

Catherine Jacobson and her son, Ben, at home in Mill Valley, Calif. His seizures have left him with very little ability to communicate, but one of his main ways of showing affection is hugging his mother’s head close to his chest. September Dawn Bottoms for The New York Times
Jacobson describes her family’s existence as akin to living under the threat of terrorism. Ben’s seizures could strike at any time. He was at high risk of what epileptologists call Sudep, or sudden unexpected death in epilepsy. “I would have done anything to save Ben,” Jacobson told me. And so one day in 2012 she found herself driving her black S.U.V. to a rundown Oakland neighborhood, past a police car, to purchase a kilo of what she had been told was CBD-rich cannabis.
Amid the current deluge of products, it now seems almost quaint that, back in 2012, after deciding to try treating Ben with CBD, Jacobson couldn’t actually locate the stuff. Other parents of epileptic children were using D.I.Y. techniques to treat their children: tinctures; cannabis-infused butter in baked goods; crushed cannabis buds in capsule form; even cannabis suppositories. Some reported positive results. Over the years, Jacobson has had many of these products tested at labs; almost invariably they contained very little or no CBD and too much THC. It has psychoactive effects, and there wasn’t much science suggesting THC could treat seizures.
In the early 1960s, a Bulgarian-born Israeli chemist named Raphael Mechoulam asked a simple question: How does marijuana make you high? The biochemistry of major psychoactive molecules from other recreationally used drugs, like cocaine and opium, was already understood. But scientists still didn’t know how cannabis worked. Mechoulam was the first scientist to map the chemical structure of both cannabidiol and delta-9-tetrahydrocannabinol, or THC. Two decades later, Allyn Howlett, a scientist then at St. Louis University Medical School, used a radioactive THC equivalent to trace where cannabinoids ended up in the brain and discovered what she would later call CB1 receptors. They were subsequently found in the kidneys, lungs and liver, too. White blood cells of the immune system, the gut and the spleen also have another type of cannabinoid receptor, known as CB2.
There is a long history of scientists gaining insight into human physiology by studying how plants interact with our bodies. Poppy flowers and the opium derived from them led to the discovery of the body’s native opioid receptors, which help regulate pain, stress responses and more. Nicotine, a stimulant found in tobacco, long used by Native Americans, taught scientists about the existence of our own nicotinic receptors, which influence neuronal excitement.
Why plants produce molecules that seem perfectly designed to manipulate human biochemical circuitry is a mystery. It could be a kind of molecular coincidence. But many plants, including cannabis, might make these molecules to defend themselves from other organisms. Modern industrial agriculture employs a whole class of pesticides based on nicotine — the neonicotinoids — meant to repel insects by over-exciting their nervous systems. Cannabinoids display antibacterial, antifungal and insecticidal properties as well.
Their ability to engage our native cannabinoid receptors may be a result of millions of years of biochemical warfare directed at would-be grazers: insects and other creatures that happen to share biochemical signaling pathways with humans. If plants target the cannabinoid receptors of other organisms to protect themselves, it follows that whatever signals those receptors evolved to receive have to be vital for these animals’ physiological health. Otherwise, why interfere with them?
[Read more about disputes over CBD’s legality.]
Mechoulam concluded that our bodies must produce their own cannabinoids — endogenous molecules that, like the native opioids and nicotinelike molecules our bodies also make, engage the cannabinoid receptors throughout the human body. In 1992, he identified the first one. Mechoulam, who is often called the godfather of cannabis research — he was a senior scientist on the Brazilian CBD epilepsy trial that inspired Jacobson — and his colleagues christened it “anandamide,” after the Sanskrit word for “supreme joy.” They suspected that the molecule played a role in the formation of emotions.
The native network of cannabinoid receptors and transmitters described by Howlett and Mechoulam is now known as the endocannabinoid system. It’s central to homeostatic regulation, that is, how the body maintains, and returns to, its baseline state after being disturbed. If a person is injured, for example, native cannabinoids increase, presumably in order to resolve the inflammation and other damage signals associated with injury. They also increase after strenuous exercise, another stressor, and some scientists have argued that they, not the better-known endorphins, are really responsible for the pleasant postexercise feeling known as runner’s high.
Endocannabinoids help regulate immune activity, appetite and memory formation, among many other functions. (Heavy marijuana use is associated with memory deficits, possibly because THC short-circuits the formation of memories.) “Perhaps no other signaling system discovered during the past 15 years is raising as many expectations for the development of new therapeutic drugs,” Vincenzo Di Marzo, an endocannabinoid researcher at the National Research Council in Naples, Italy, wrote in 2008, in the journal Nature Reviews Drug Discovery. But realizing such medical benefits has proved trickier than once imagined.
When scientists at the French pharmaceutical company Sanofi-Aventis (now Sanofi) understood that THC could whet a user’s appetite, they created a weight-loss drug that blocked CB1 receptors, hoping to suppress appetite. Rimonabant was first released in Europe in 2006. Two years later, regulators pulled it from the marketplace because of its severe side effects, including depression and suicidal behavior. The episode seems to exemplify endocannabinoids’ importance to our sense of well-being and the difficulty of manipulating them therapeutically. Attempts to increase native cannabinoids with synthetic drugs have fared no better. In 2016, French scientists halted a study of a drug designed to boost endocannabinoids. For reasons that remain unclear, six patients who took the medicine, meant to treat pain, were hospitalized. One died.
And yet, for millenniums people have used cannabis itself with relatively few side effects. (These can include dry mouth, lethargy and paranoia.) THC hits CB1 and CB2 receptors, but how CBD works is less clear. It seems to interact with multiple systems: increasing the quantity of native cannabinoids in the human body; binding with serotonin receptors, part of the “feel good” molecular machinery targeted by conventional S.S.R.I.s; and stimulating GABA receptors, responsible for calming the nervous system. With more than 65 cellular targets, CBD may provide a kind of full-body massage at the molecular level.
This biochemical promiscuity is one reason CBD seems so medically promising, according to Yasmin Hurd, a neuroscientist at Mount Sinai, in New York. Modern neuroscience often tries to target one pathway or receptor, Hurd told me; that approach is easier to study scientifically, but it may not address what are often network-wide problems. “The brain is about a symphony,” she says. And CBD, she suspects, can “bring the entire symphony into harmony.”

Various products that have been advertised as containing CBD.Photograph above with products that have been advertised as containing CBD. Top row: Meringue cookies, Elite Hemp Products; lollipop, Nova Blis; golden milk powder, Supergood; marshmallow, The Marshmallowist. Second row: skin oil, Herbivore; gummy bears, Just CBD; dog biscuits, Medipets; popcorn, Diamond CBD. Third row: Rainbow gummy, Diamond CBD; mints, Tillmans Tranquils; suppositories, Foria; mascara, Milk Makeup. Fourth row: gumdrops, Lord Jones; chocolate, Grön CBD; gummy candies, Just CBD; bamboo extract, Meds Biotech; melatonin, Meds Biotech; gel capsule, Lord Jones. Jamie Chung for The New York Times. Prop styling by Anna Surbatovich.
Cannabis has been used medicinally for thousands of years in Asia, where it was probably first domesticated before traveling to, among other places, Africa. It was almost certainly introduced multiple times to the Americas, first from Africa to South America through the slave trade — in Brazil it’s still known by an African name, diamba — but also to the Caribbean. Indian indentured laborers probably brought it to Jamaica, where it’s called by an ancient Indian name, ganja.
White Americans also had some history of using cannabis in tinctures. In the early 19th century, an Irish doctor working in India, William Brooke O’Shaughnessy, had observed that cannabis was used extensively in Indian medicine. He began experimenting and found it quite efficacious not only for infantile seizures but also rheumatism and spasms caused by tetanus. O’Shaughnessy usually gets the credit for introducing the plant to the English-speaking world, but while he popularized its use in Britain, he was not the first European to bring it back to Europe. Garcia Da Orta, a Portuguese physician, had, after living in India, written about cannabis as medicine in the 1500s.
After O’Shaughnessy published his treatises on the plant, its use spread rapidly among physicians. By the late 19th century, cannabis was an important component of British and American physicians’ pharmacopoeia. (Researchers suspect that these older cannabis cultivars, and the tinctures made from them, probably contained much less THC and much more CBD than modern varieties.) Of course, hemp, a variety of cannabis bred not for consumption but for the fiber that goes into ropes and sails, among other things, had been an important crop in Europe and the Americas for centuries. George Washington grew it. The English word “canvas” derives from the Greek kannabis.
But in the late 19th century, our ancient relationship with this plant began to fray. In 1930, Harry Anslinger, a former official at the Bureau of Prohibition, assumed a new job running the Bureau of Narcotics. The Mexican Revolution that began in 1910 had led to waves of immigrants crossing into the United States. Whereas many Americans took their cannabis orally in the form of tinctures, the new arrivals smoked it, a custom that was also moving north from New Orleans and other port cities from which African-Americans were beginning their own migration.
Anslinger disdained Mexican-Americans and African-Americans. He loathed jazz. Modern scholars argue that his demonizing cannabis both justified his position and provided a way for him to gain legal leverage over peoples he despised. The high cost paid by people of color, once he had begun what we now call “the war on drugs,” may not have been an incidental byproduct of his efforts but an unstated goal from the start. His protestations still echo today. Cannabis made people crazy, violent and prone to criminal behavior, Anslinger said.
Yet when 30 American Medical Association members were surveyed, starting in 1929, 29 disagreed with claims about the dangers posed by cannabis. One said the proposals to outlaw it were “absolute rot.” But the hysteria Anslinger helped stir up worked politically. In 1937, Congress passed the Marijuana Tax Act. High taxes made cannabis much more expensive and difficult to obtain decades before President Nixon — scientists of his era disagreed with him, too, about marijuana’s supposed dangers — signed the Controlled Substances Act of 1970. A plant that people had used medicinally for thousands of years was now driven underground.
Jacobson’s dealer in Oakland seemed to be selling harder stuff as well, which made her very nervous. But her impression was that he was having a difficult time selling this particular product — kilos of California-grown cannabis — precisely because it wouldn’t get anyone very high. With her black-market stash in hand, Jacobson entered what she calls her R.& D. phase. As suspected, the cannabis she had acquired illegally in Oakland was high in CBD and low in THC. She set up a lab in her garage — and then proceeded to fail miserably, for months, to extract anything of much use. Only under the tutelage of two University of California, Davis, scientists did she make progress. The technique she developed required heating cannabis plants in ethanol to extract the cannabinoids. Next, a machine that created a vacuum sucked the green-tinted liquid through a tube filled with carbon powder. The molecules in the extract moved through the powder at different speeds, depending on their weight and other characteristics, yielding different “fractions” that she could test for CBD and THC content. Then she heated the resulting green solution until the alcohol evaporated, leaving a green paste. It took her about six months to perfect the process. Finally, nearly a year after starting, she had a cannabis extract that was high in CBD and lacked measurable THC.
Ben improved somewhat after taking it, but it was another boy with severe epilepsy, 11-year-old Sam Vogelstein, who responded most significantly. Jacobson and Sam’s mother, Evelyn Nussenbaum, had met and become close friends as together they sought a safe and reliable source of CBD for their children. But now Jacobson felt a different sort of pressure. Making the medicine was difficult. Despite all that she had learned, some batches of her extract were unusable. And who knew if the source material she was buying illegally would remain available? If this was to be their sons’ medicine, Jacobson wanted a pharmaceutical-grade product that she could always obtain.
Across the Atlantic, Geoffrey Guy, the founder of a company called GW Pharmaceuticals, had successfully brought one cannabis-derived medicine, called Sativex, to market in Britain and other European countries. The first such medication permitted by a government, it was approved to treat the symptoms of spasticity (as well as pain) caused by multiple sclerosis, a progressive autoimmune disease of the central nervous system. It contained both CBD and THC. Guy was intrigued when, through a mutual acquaintance, a California family seeking CBD to treat epilepsy reached out to him — Evelyn Nussenbaum and her son Sam.
Guy agreed to treat Sam. Jacobson had her extract analyzed and the results sent to Guy. In December 2012, Sam and Nussenbaum flew to London for two weeks to try a purified CBD drug that Guy had created just for him. He started with a small dose and, as it was gradually increased, his seizures faded. Before his trip, Sam was taking three conventional medications and still having dozens of seizures daily. But after he reached the highest daily dose of CBD — 250 milligrams — his seizures stopped almost entirely for a week. He became more articulate and coherent than he had been since he was 5, when his condition took a turn for the worse. He rode a zip line in Hyde Park, took the subway and did other things that Nussenbaum had always avoided for fear that he would seize and hurt himself. Nussenbaum describes that week as “Twilight Zone weird,” as if she had entered a parallel dimension.
The high cost paid by people of color from what we now call “the war on drugs,” may not have been an incidental byproduct but an unstated goal from the start.
[Read about how China is cashing in on the cannabis boom.]
After he returned to the United States, it was six months before Sam could take Guy’s extract again. Medical marijuana is illegal under federal law — its designation as a Schedule 1 drug means it is considered to have a high potential for abuse and without any known medical application — but Sam gained access to Guy’s extract through the F.D.A.’s compassionate-use program, which makes still-unapproved drugs available to patients with serious conditions. (In 2015 Sam’s father, Fred Vogelstein, a journalist, detailed Sam’s story in Wired magazine. In 2010, he also wrote in this magazine about using a ketogenic diet, since discontinued, to control Sam’s epilepsy.) With a petition from a U.C.S.F. epileptologist, Roberta Cilio, who was the doctor for both boys, Ben also received the medicine through the F.D.A.’s compassionate-use program. It helped, Jacobson thought, particularly with the most severe fits, which caused him to lose consciousness. But he was by no means seizure-free.
Jacobson and Nussenbaum knew many other families struggling with epilepsy. They were aware of the suffering and desperation of those who belonged to this “club that no one wanted to join,” as Nussenbaum puts it. Many parents lacked the resources and connections they had. Everyone should have access to the drug that had so helped Sam, they thought. But that meant the F.D.A. would have to approve CBD for epilepsy. For that to happen, real trials had to take place. And given the fraught political history of cannabis in the United States and the skepticism they would most likely face, Jacobson knew she would need top epilepsy experts to conduct those trials.
The D.E.A.’s classification of cannabis as a Schedule 1 drug, alongside heroin, peyote, ecstasy and LSD, has made it difficult for American scientists to study. Much of the research into its therapeutic potential comes from other countries, including Brazil. In the 1970s, Antonio Zuardi, a neuroscientist at the University of São Paulo, began looking into how cannabinoids affect mental states. Large quantities of THC could cause anxiety and paranoia in volunteers, he discovered, but CBD could attenuate the anxiety-provoking and psychoticlike effects of THC. Later studies by Zuardi and his colleagues showed that a large dose of CBD, when given to volunteers who feared public speaking — that is, who suffer from social anxiety — blunted the flight-or-fight response, measured by increases in heart rate, blood pressure and skin conductivity, prompted by having to address others. These were small studies, and the amount of CBD involved, which was 600 milligrams in the social-phobia study, is greater than what users might consume these days in some CBD gummies, for example, but relieving anxiety is nonetheless one of the most widely reported reasons people use CBD.
CBD may also have antipsychotic properties. In susceptible individuals, its sister cannabinoid THC can, in high doses, induce psychotic symptoms, and heavy marijuana use early in life has been linked to an increased risk of developing psychotic disorders, possibly because it alters brain development. But just as Zuardi discovered that CBD can blunt anxiety, scientists at King’s College London have found evidence that CBD can lessen the psychosis-producing effects of THC and maybe help treat schizophrenia, a disorder whose main symptom is psychosis. The scientists are now testing CBD as a prophylactic to prevent schizophrenia from even emerging.
Many of those who develop schizophrenia first pass through a “prodromal” phase. They suffer from delusions, but they’re still aware that these experiences aren’t real and often seek psychiatric help. A single 600-milligram dose of CBD given to these patients, scientists at Kings College London have found, can partially normalize regions of the brain that have been shown in fMRI visualizations to become dysfunctional during schizophrenic episodes.
A follow-up study will prophylactically treat a large group of these patients thought to be teetering on the edge of psychosis. Current schizophrenia treatments merely attempt to manage the disorder once it has already emerged. A medicine that slows or prevents the disease from taking root altogether, almost like a vaccine, would address a huge unmet need. “If it works, it will be a revolution,” José Crippa, a neuroscientist at the University of São Paulo who is involved in the project, told me.
It’s reasonable to ask why the CBD naturally present in cannabis doesn’t protect recreational users from the negative effects of THC. In older varieties, where the CBD-to-THC ratio was closer to 1-to-1, maybe it did. But today’s strains typically contain about three times as much THC as the cannabis smoked recreationally even as recently as the 1990s, while CBD concentrations have fallen by about half in the same period, according to a recent University of Mississippi study on black-market marijuana. And precisely because the proportions between the two cannabinoids have become so skewed — the ratio of THC to CBD has risen to 80 to 1 from 14 to 1 in two decades — lots of modern cannabis is potentially much more toxic for the brain, says Hurd, who is the director of the Addiction Institute at Mount Sinai.
Some years ago, Hurd discovered that THC could, as opponents of marijuana legalization have long maintained, prompt heroin-seeking behavior in rodents, acting as a proverbial “gateway drug.” But she also found that CBD reduced drug-seeking behavior, which led her to change the focus of her work. Now she studies how CBD could help opioid addicts kick the habit.
Hurd’s research, replicated by others, indicates that CBD might help recovering opioid addicts avoid relapse, perhaps the greatest challenge they face. She’s not sure why but suspects that by reducing anxiety and craving — major triggers of relapse — CBD helps patients stay the course. And because it’s not habit-forming, like other anti-anxiety medications, CBD might be a badly needed new weapon with which to fight an epidemic that claims more than 130 lives daily in the United States.
THC may also have therapeutic uses, particularly in treating the pain that often puts people on a path leading toward opioid addiction. Several studies have found that cancer patients need fewer opioid painkillers if they’re also using cannabis. And opioid-related deaths have declined in states that legalized medical cannabis, suggesting that people who have access to less-addictive options for pain management may not be as likely to become hooked on opioids.
CBD might be a badly needed new weapon with which to fight the opioid epidemic that claims more than 130 lives daily in the United States.
Other possible applications of plant-derived cannabinoids could be just as groundbreaking. Scientists at New York University are studying CBD as a possible treatment for autism spectrum disorders. Spanish researchers are testing both THC and CBD on an aggressive brain cancer called glioblastoma. Israeli scientists have found that CBD can lessen the incidence of graft-versus-host disease in bone-marrow transplant patients, presumably because the cannabinoid calms the immune system and deters it from attacking the patient.
How could one family of molecules help so many maladies? The most obvious response is that they might not; all this research is preliminary and might not pan out. But scientists often propose a counter-explanation: Many chronic disorders, even though they seem distinct, are characterized by dysfunction in the same few pathways. Inflammation and oxidative stress, for example, occur in schizophrenia, metabolic disorders, heart disease and other ailments. The therapeutic magic of CBD and, in some cases, THC — and maybe some of the more than 100 other cannabinoids in cannabis — may come from the ways that, by tweaking the endocannabinoid system, they push the body away from disease toward the unruffled state scientists call homeostasis.
There are other examples of a single drug being able to help meliorate a variety of conditions. We know aspirin as a treatment for fever and headache, for example, but in low doses it is also used to reduce the risks of stroke, heart attack and pre-eclampsia in pregnant mothers; it even figures as an adjunct treatment for schizophrenia. Aspirin has its own downsides — an elevated risk of bleeding, for instance — but like CBD, its broad utility may be partly explained by its anti-inflammatory effects. Like CBD, aspirin is derived from a plant. The active ingredient in aspirin, salicylate, was first extracted from willow bark and was a folk remedy for thousands of years before scientists finally made a pill from it in the late 19th century. Folk medicine, for all its associations with old wives’ tales, has yielded important medical discoveries in the past, and it may well do so again.
In early 2013, just a few weeks after Sam Vogelstein returned from Britain, Catherine Jacobson organized a brainstorming session at N.Y.U., which included Geoffrey Guy, epilepsy researchers and a consultant with a D.E.A. background, in order to figure out how to make F.D.A.-sanctioned trials happen. What followed the meeting surpassed Jacobson’s expectations. The F.D.A. first expanded the ability of doctors to prescribe CBD and then fast-tracked the approval process. The neurologists who ran the trials included Orrin Devinsky from N.Y.U., Elizabeth Thiele from Harvard and Eric Marsh from the University of Pennsylvania.
In June 2018, just five years after that meeting — an instant in drug-development time — the F.D.A. approved GW Pharmaceutical’s CBD extract as a treatment for two rare forms of epilepsy, Lennox-Gastaut syndrome and Dravet syndrome. And three months later the D.E.A. rescheduled this first CBD drug (but not THC) to Schedule 5, meaning it was now considered to have low potential for abuse.
The drug, called Epidiolex, is not the first cannabis-related drug on the market. Marinol, used to suppress nausea and stimulate appetite, contains THC. But Epidiolex is the first drug that contains only CBD and the first one derived directly from the cannabis plant itself. (The THC in Marinol is synthetic.) As a new class of medicine, Thiele told me, it’s important for the reasons Jacobson recognized years ago: It hits different pathways than do currently available epilepsy drugs, thereby expanding the available treatments for difficult-to-treat childhood epilepsies.
Epidiolex is also noteworthy for its unusual history. Drugs are typically developed in the lab and go through trials before reaching patients. But in the case of Epidiolex, two mothers of epileptic children experimented on their own sons and then helped push a version of what they discovered into the F.D.A. pipeline. “In the modern era, it’s certainly the most striking example of a drug that has gone from patient use to drug development,” Ken Mackie, a neuroscientist at Indiana University, told me. And it’s unlikely to be the last such example. Because so many people already use cannabis and think it helps, patients might be, in effect, pioneering new uses through self-experimentation.
This trend concerns many physicians, who worry that patients may be deluding themselves, but some scientists interested in cannabinoids have begun to look to “vernacular” applications for clues about what to study formally. Users, meanwhile, look to the published literature as Jacobson did for guidance on how to use cannabinoids. The end result is that cannabis science and vernacular cannabis use exist in an uneasy symbiosis. “It’s this completely unprecedented situation,” Jacobson says. “I don’t think there’s another product out there that’s a wellness drug, a pharmaceutical drug for severe disease and a recreational drug.”
CBD is generally considered safe, even at the high doses tested so far — and the quantities in chocolates, teas and other edibles tend to be far below the concentrations tested experimentally. But given that cannabis regulations vary from state to state, scientists and patient advocates worry that consumers may not be getting what they think they’re getting.
Still, many who have direct experience with CBD, including a few scientists, do not think it should be available only by prescription. They point out that long before the 1970 Controlled Substances Act, which made marijuana illegal, people used the plant medicinally. Cannabis should not only take its place as an F.D.A.-approved drug, they contend. It should also reclaim its role as a folk remedy.

From left: Margarita Sanchez, Ben’s nanny, Ben and Catherine at home. Ben wears a strap to prevent him from falling when he has his seizures. September Dawn Bottoms for The New York Times
If there is a Patient Zero in the vernacular cannabis movement, that person is a girl in Colorado named Charlotte Figi. Her seizures began at 3 months, as Ben Jacobson’s had. Doctors diagnosed Dravet syndrome, in her case caused by a spontaneous genetic mutation. By the time she was 5, she was wheelchair-bound, receiving sustenance through a feeding tube, seizing about 350 times per week, and on several occasions she had to be shocked back to life after her heart stopped. Doctors once recommended a medically induced coma just so her body could rest.
In 2011, as a last resort, Charlotte’s mother, Paige, gave her a CBD-rich extract, acquired from a local grower, via feeding tube. (Medical cannabis has been legal in Colorado since 2000.) The seizures almost entirely disappeared. Word of this success spread through the network of medical-marijuana professionals, and early in 2013, someone called on behalf of the CNN medical correspondent Sanjay Gupta. Gupta, who is a neurosurgeon, had previously argued against the legalization of medical cannabis, but he now wanted to do a show on it. After much discussion, Paige Figi and Joel Stanley, the Boulder-based cannabis grower who had produced the extract for Charlotte, decided to invite Gupta to tell their story. If it came from a skeptic of his standing, people might actually believe it.
Gupta visited the Figi home, watched old videos of Charlotte seizing, looked at family photos, and saw the Charlotte before him as a playful little girl of 6. At one point, Paige Figi told me, Gupta, who has daughters of his own, requested that the cameras be turned off, and cried.
He came away a convert, convinced of medical cannabis’s effectiveness. And the show, which aired in August 2013, catapulted Charlotte’s story to national prominence and Figi into a new, unexpected phase in her life. Within days of Gupta’s report, people began showing up at the Figi family’s door, desperate parents of epileptic children from elsewhere in the country who picked up and moved to Colorado in the hope of acquiring medical cannabis. Figi fed them. Some stayed a few nights. One family ended up living with them for a year. A community began to coalesce in Colorado Springs, made up of epileptic children and their families.
Around the same time, Figi, Stanley and Heather Jackson, another mother whose epileptic son had benefited from CBD, founded a nonprofit called Realm of Caring. It helped families relocate to Colorado and offered them advice on how to negotiate the state’s medical- cannabis environment.
This was also a period of some tension and confusion. Stanley couldn’t keep up with the surge in demand. He kept long waiting lists of hopeful parents. Westword, a Denver-based paper, published a story in which parents — some of whom didn’t seem to realize that Realm of Caring did not provide cannabis products — vented about feeling ignored. One father, whose very sick son had benefited from Stanley’s cannabis extract but then suddenly died, wondered obliquely if he had contributed to his child’s death. (Stanley’s company responded with a statement saying that elements of the Westword story were inaccurate.)
Figi and Stanley eventually left Realm of Caring to avoid conflicts of interest. In 2017, the F.D.A. sent a letter to Stanley and Realm of Caring warning them to stop making medical claims about treating specific disorders. (Both say they updated their websites.) Today, Stanley is the chairman of Charlotte’s Web, a company named after Charlotte Figi. Last fall, the business went public in Canada; it projects more than $120 million in sales this year, more than triple its 2017 sales.
Where Jacobson and Nussenbaum saw their role as helping a cannabis-derived drug get F.D.A. approval, Figi focused on legislation, becoming a kind of CBD ambassador. She testified before State Legislatures and helped draft a 2017 House bill that, if it hadn’t died, would have legalized CBD nationally.
Figi, who says she switched her party affiliation from Republican to Democrat after Donald Trump was elected president, even considered running for elected office and making access to CBD part of her platform. Given CBD’s many therapeutic benefits, she reasons, the cannabinoid should be legally available for use without prescription. And that access should not depend on whether recreational cannabis is also legal. “I’m just trying to help these kids,” she told me this past winter. “We can do something for them now. Why hold them hostage?”
One reason some physicians look askance at the vernacular cannabis movement is that it can, in its sometimes quasi-religious devotion to the plant, seem almost cultlike. Kristen Park, an epileptologist at Children’s Hospital in Colorado, told me that after Gupta’s CNN story aired, patients from around the country seeking medical cannabis inundated the hospital. She had no data at that point on its efficacy and did not recommend it. The Epidiolex trials have provided some evidence of effectiveness, Park told me, but she still frets over the phenomenon. Sometimes parents of patients refuse established epilepsy treatments in favor of cannabis products, she says, because these are perceived as somehow natural and thus superior to standard medicines. Other parents insist cannabis is helping their children when, in her view, it clearly isn’t — and they refuse to stop using it when they should move on to other treatments. “Because of all the hype, people somehow think this is a cure-all and a treatment that will fix everything,” she told me. What’s lost on many, she says, is that even if CBD helps, it’s still just another drug, and no drug works for everyone all the time.
‘Because of all the hype, people somehow think this is a cure-all and a treatment that will fix everything.’
Nor are most drugs completely free of side effects. In the standard drug-approval process, observed side effects are noted on the packaging. If new ones show up after F.D.A. approval, they can be added later. As Ken Mackie, from Indiana University, told me, there’s no mechanism to do this in the vernacular movement, no central repository of interactions and side effects.
CBD has known side effects. Elizabeth Thiele, the epileptologist at Harvard, says that some children, for reasons that aren’t clear, undergo mood changes on some nonprescription CBD oils. (These issues might be caused by different cannabinoids or terpenes, another type of biologically active molecule produced by plants.) CBD can also interfere with how quickly the body breaks down other medications.
The greatest concern, however, and one I heard repeatedly from parents and physicians, is quality control. In 2015, the F.D.A. found that many CBD-labeled products actually contained very little CBD. It sent out a flurry of letters warning companies not to make medical claims. Two years later, a study published in JAMA documented that, in 84 products sold online, 26 percent had less CBD than advertised and 43 percent had more. And the cannabis plant can absorb toxic substances like heavy metals or pesticides as well as carry infective agents. In 2017, a California man undergoing chemotherapy, whose immune system was weakened, died from a fungal infection that his physicians suspect he acquired from the cannabis he smoked to ease his symptoms.
Last year, California legalized recreational marijuana and phased in a series of stringent quality controls, including tests for various microbes, pesticides and heavy metals. Customers who buy cannabis from licensed California dispensaries can now be reasonably confident that they’re getting what they think they’re buying and that it’s safe to consume. This goes for some other states as well.
Even as a wave of entrepreneurs has founded companies already worth millions in what’s often called “the green rush” — the explosion of cannabis-related business — many people of color remain incarcerated for marijuana-related crimes. Some states and cities are moving to correct this. For example, last year Denver’s mayor announced that more than 10,000 convictions for low-level marijuana crimes, going back to 2001, would be eligible for expungement.
At the same time, confusion about the federal legality of CBD-related commerce remains widespread. The 2018 Farm Bill legalized hemp, a low-THC, potentially high-CBD variety of cannabis, meaning that CBD from hemp is now theoretically legal nationwide. But there’s a wrinkle: The F.D.A. says that because CBD is also an approved drug (Epidiolex), the cannabinoid can’t be considered, as some argue it should be, a nutraceutical or dietary supplement. The companies that ship CBD products across state lines — an activity subject to F.D.A. enforcement — may be doing so illegally. Yet even though the F.D.A. has the authority to clamp down on CBD-related products and interstate commerce, it can choose not to do so. F.D.A. enforcement action depends on, among other things, available resources and the perceived threat to public health. (An F.D.A. spokesman declined to comment.)
J. Michael Bostwick, a psychiatrist at the Mayo Clinic, in Rochester, Minn., who has written about cannabis, calls the hodgepodge of conflicting rules regarding cannabis “idiotic.” He told me that even physicians willing to oversee patient cannabis use, who live in states where it’s legal, can be reluctant to do so because it remains illegal under federal law. A doctor’s license to practice medicine comes from the state, but because the license that allows doctors to prescribe medicine is federal, involvement with cannabis could lead to revocation of that license. “There’s a lack of clarity about what playing field we’re on,” Bostwick says.
One obvious solution to the uncertainties around legality, quality and safety of CBD products would be to force all CBD into the F.D.A. drug-approval pipeline, making it a prescription drug only. Somewhat surprisingly, Catherine Jacobson does not want that to happen. Her thinking on this issue has evolved, she told me. Early on, she thought all medical cannabis products should go through the F.D.A.’s approval process. But she realized that her primary concern, quality, could be assured without this expensive, time-consuming undertaking. In Germany, for instance, doctors have been able to prescribe cannabis since 2017, and patients get a pharmaceutical-grade product, because a federal agency oversees the medical-marijuana industry.
Jacobson, who lives in Mill Valley, Calif., now works remotely for a Canadian-based company that has also, she thinks, solved the quality problem. She’s vice president of regulatory-and-medical affairs for Tilray, which produces medical-grade cannabis products and flowers and ships them wherever they’re federally legal (and so not to the United States).
What about the uncertainties over whether CBD works for a given illness? Jacobson didn’t necessarily see the lack of evidence of effectiveness as a problem. When it comes to diseases like intractable epilepsy, she said, doctors often do their own experimenting. They try standard treatments first, but when those fail, as they did in Ben and Sam’s cases, they turn to drugs that might not be approved for epilepsy or even for children. Some of these drugs might cause severe side effects, including fits of rage or sedation so extreme that, as one mother described it to me, “the light goes out” in a child’s eyes.

A bottle of Tilray’s C100, developed for treating seizures. Jamie Chung for The New York Times
Jacobson and other parents I spoke with argue that in difficult medical cases, doctors are already tinkering with potentially toxic drugs, so why can’t they — the parents or the patients — experiment with a less-toxic product? Why can’t everyone? Scientists could search for signals on what to study in this sea of self-experimentation. Realm of Caring, still run by Heather Jackson, is already doing this in partnership with academic researchers, sharing data from a 55,000-person registry that includes information on what people are using cannabis for and what side effects and benefits they see.
One scientist is doing something similar with herself as a subject. In 2017, Diana Martinez, a professor of psychiatry at Columbia University, found out she had breast cancer and started chemotherapy with taxane, a class of drug known to cause nerve damage. Martinez began to hear ringing in her ears, feel pins and needles in her hands and lose feeling in her lower limbs. Eventually she could barely swallow, started to fall while walking and ended up concussed. In up to 80 percent of women who use taxane, these symptoms persist. Martinez decided that even if the drug helped her beat the cancer, the symptoms, which were likely to get worse, were unendurable. Over her family’s objections, she quit the chemo.
Then a colleague reminded her that she had always wanted to study CBD for nerve pain. Why not try it herself? Martinez ordered CBD extract from a place in Colorado that seemed reputable — Charlotte’s Web, it turned out. After about six weeks on the oil, the ringing in her ears disappeared and the other symptoms began to fade. “I could swallow,” she told me. “I could walk down the street, type on a computer. It was gone. It seemed fairly miraculous. It still does.” She completed the chemo, this time with fewer side effects.
Martinez, inspired by her own experience, has since started a trial with her colleague, a neurobiologist at Columbia named Margaret Haney, that will target taxane-induced neuropathy in breast-cancer patients with a pill containing both THC and CBD. The cannabinoids may work better together for some conditions, especially when pain is a factor. (Jacobson’s continued behind-the-scenes influence is evident here as well. Tilray created the formulation for Martinez’s trials.) If it helps, the cannabinoids might save lives not because they cure cancer — although others are studying that possibility as well — but because they might assist women in completing otherwise intolerable courses of chemo.
And the only reason she’s pursuing this line of inquiry, Martinez points out, is that a quality, CBD-rich hemp extract was readily available when she needed it. “I’m grateful for Charlotte’s Web,” she told me. Prospective users need to do their homework and research product quality, but “when people want to take CBD,” she added, “I’m like, ‘Go for it.’ ”
CBD is not always an unqualified success, even in the best-known case studies. For Sam Vogelstein, the inspiration behind Epidiolex, it helped control his seizures for years, limiting them to around six per day. But in the fall of 2015, Sam began suffering from a new type of seizure. These were more severe, causing him to fall to the floor writhing, which hadn’t occurred in the past. “You instantly understand why people used to say that people who have epilepsy are possessed by the devil,” Fred, Sam’s father, told me, “like some external force has taken control of this person.”
Higher doses of Epidiolex didn’t help, so Sam’s doctor, the neurologist Roberta Cilio, recommended an anti-seizure drug called Depakote. He had taken it before, without benefit, but this time, in combination with Epidiolex, it worked wonders: Sam has been completely seizure free for more than three and a half years. He’s a tall, lanky 17-year-old who likes to fence, run and engages in “normal aggravating boy teenager stuff,” his father says — and “cause for celebration,” both parents say.
Ben Jacobson’s condition is more ambiguous. In an effort to stop the seizures, doctors surgically removed half of Ben’s parietal lobe in 2015, but the procedure didn’t mitigate the epilepsy. His doctor, Cilio, didn’t think the Epidiolex was aiding him, either, and recommended he stop taking it. Jacobson, who like many mothers of epileptic children keeps a detailed diary about seizure activity, disagreed. By her count, the number of Ben’s seizures had declined by 40 percent while on Epidiolex, particularly the severe grand mal seizures that caused him to stop breathing.
This disagreement between doctor and mother prompted Jacobson to find a new neurologist who, she told me, took one look at Ben and told her to do whatever she felt might help. Except for a few breaks, Ben, who’s now 10 and can’t walk unaided, has remained on Epidiolex, but his prognosis isn’t great. “He’s still going downhill,” Jacobson told me. “His life expectancy is short enough that we don’t like to think about it.”
Charlotte Figi, now 12, continues to be almost entirely seizure-free. She’s developmentally delayed, Paige Figi told me. And she suffers from osteoporosis caused, Figi thinks, by the high doses of steroids she took to control seizures at a young age. But she is otherwise a happy, playful girl, Figi says. And what Figi discovered about CBD on Charlotte’s behalf came in handy for Charlotte’s fraternal twin sister, Chase.
Two years ago, Chase, who until then had exhibited no problems, began to have seizures out of the blue.
Figi didn’t even bother with allopathic drugs this time. She turned straight to the Charlotte’s Web CBD extract, and the seizures stopped. “If I hadn’t done this,” Figi says — that is, experiment with CBD extracts on Charlotte — “Charlotte would be dead. And Chase would now be starting all those drugs.”
Meanwhile, as the science inches forward, CBD has become a pop-culture phenomenon. Kim Kardashian recently hosted a CBD-themed baby shower. In April, Carl’s Jr. tested a CBD-infused burger in Colorado.
Some scientists are concerned by how far the CBD craze has moved beyond the science. But Staci Gruber, associate professor of psychiatry at Harvard Medical School, does not think the two are necessarily in conflict. This might seem odd, given her work. She has found that recreational users, particularly those who begin using cannabis earlier in life, exhibit some cognitive difficulties and altered brain structure and function.
In 2014, Gruber started the Marijuana Investigations for Neuroscientific Discovery, or MIND, program to examine the effects of medical cannabis, and so far, she has found exactly the opposite in people who use cannabis as medicine. Their cognitive function appears to improve over time and preliminary evidence suggests that, after initiation of medical-cannabis treatment, their brain activity begins to normalize.
Although Gruber is not certain what accounts for the contrasting effects, she has several theories. Seeking a euphoric high, recreational users often gravitate toward products higher in THC. Medical patients, meanwhile, want to control symptoms and may thus seek whole-plant products that not only contain more CBD than what recreational users typically encounter but also other potentially healthful cannabinoids. Medical users tend to be older, too, and some evidence suggests that THC is less toxic to older brains than younger and may in some cases benefit older brains.
Gruber has likewise observed that medical cannabis patients tend to reduce their use of conventional medications over time, which might itself be beneficial to brain structure and function. Whatever the explanation, Gruber believes greater scientific engagement with the CBD phenomenon is as important as more careful regulation. “People have been using cannabis forever,” she told me. “The question now is, How do we as scientists catch up?”
Moises Velasquez-Manoff is a contributing Op-Ed writer for The Times. He last wrote for the magazine about tick-borne meat allergies.
Gummy Bear image: Concept and diagram by Paul Sahre. Photo illustration by Jamie Chung. Prop styling by Anna Surbatovich.