by Michael Bailey | Jun 1, 2020 | Health & Medicine, Psychology, Society and Culture |
Connecticut is but one single solitary state that has clamped down on public activity, business operations, and asserted itself in cautious messaging to its residents for the last two months.
There are 49 other states in our country. Many have done the same, if not more. Some have done less. Still other state governments, in doing little from the start, or acting late, have cemented their reputation as lands of questionable judgment.
I am fortunate to live in a community with a leading educational institution that publishes articles such as these to remind readers to stay vigilant, and stay smart. But, there’s more to it than that. People can not wait for articles like this to magically drop from the sky into their lap. We need to proactively follow writers and dispensers of information that are interested in our public health and knowledge scores. Not politics and commerce interests. I “choose” to subscribe to, and trust, posts and information lines like these.
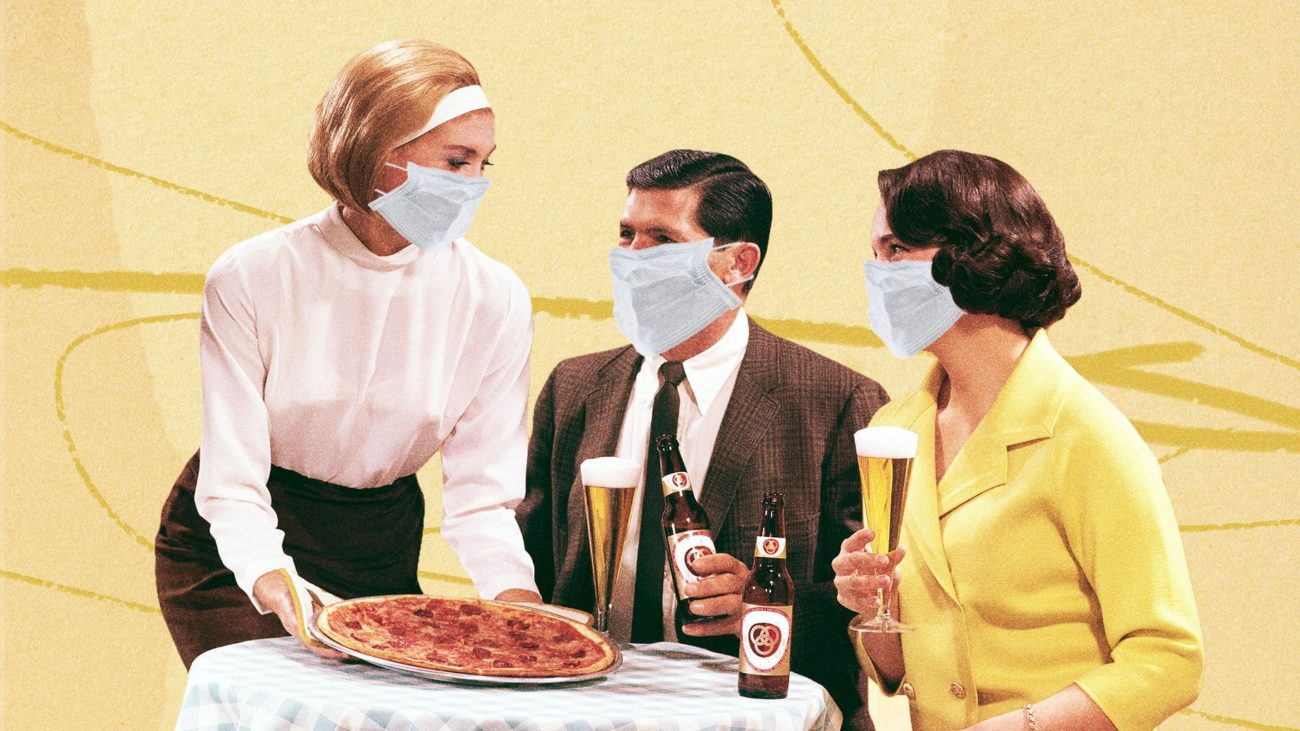
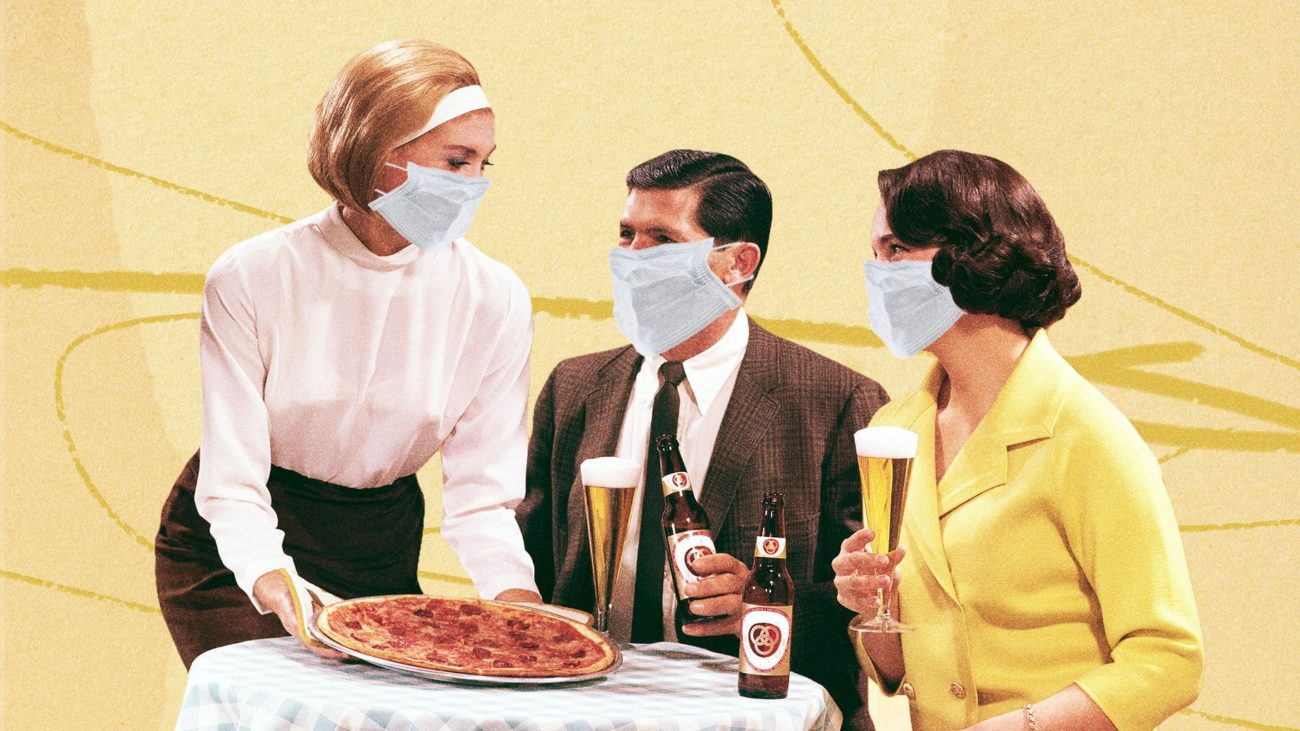
As I drove through a couple neighboring towns in New Haven this past “re-opening” week, I noticed some things that changed literally overnight. Restaurants have set up outdoor tables wherever they can in hailing distance of wait staff. At one of these outdoor table, sat four diners kicking back in their summer shorts, golf shirts, and sleeveless dresses, crowing, laughing, having a good ol time while throwing back beers as if all were finally as it should be. I couldn’t help thinking this group, as many others, felt it should’ve been this way all along since early April. Just down the road, at a popular tequila bar, sitting at a single hi-top table positioned directly on the sidewalk, just aside of its main entrance, and inarguably, encroaching on foot traffic passing by, sat five people elbow to elbow indulging in happy hour. Over the next days more of these sightings were obvious. People sitting together in parties of four, or five, just barely six feet apart from more tables with other people having food and drinks brought out to them. In virtually all of these scenarios, the tables were directly on the sidewalk, sometimes, not always, separated by a waist high iron or wooden fence, where pedestrians were walking by close enough to pick a french fry off a table.
I know I’ve got company who would find both these scenes unsettling at this time and place. I also know there are others who are next in line to grab a table and damn the torpedoes. Thus is the pervasive contradiction of human behavior which opposes as much as it embraces, sometimes with careful deliberation, sometimes with thoughtless impulse.
Ever since this viral mess reached its second month in April, no less June, there’s been as much discussion about the social casualty of isolation, as there has been about the economic and health casualties. There have been so many stress points trying to reconcile these very different vested interests, that the conversation inevitably degrades into conflict, judgment, and lost tempers among people who might not otherwise be colliding in their lives.
The question was glaringly obvious. How is it possible to prioritize these three distinct focal points affecting human beings in such direct and powerful ways, each of which has its own intertwined impact on the other? To me, it is almost impossible. Where does impossible leave us?
It became clear to me months ago, and remains so, that these challenging times are at the top of the list of what organized central government was conceived to address. For instance, conceiving and executing comprehensive plans to address major issues impacting our economy, our public health, and our societal well being. Sadly, during this time, it also became clear, that our federal government would fail us spectacularly in this fundamental mission.
So, are we back to impossible after all? I don’t believe it is impossible IF reality is faced, sacrifices are made, and the inevitable losses are accepted. If we as individuals, as groups, as calm, meditative thinkers, with respect for ourselves, and life around us, gather credible information about this public health risk, and act responsibly, we can salvage the best outcome for ourselves. Even given inevitable losses, there’s a control for a better or worse outcome. Its horrible. Its been horrible. People died. More will die. Business closed. More will close. People lost jobs. More will lose jobs. Still, I ask, you want better, or worse?
Covid -19 is still here. It still gets people sick, and it still kills. As true as it was in February and March, it is true now. Any single action by any given individual in the public space has the potential to trigger a transmission contact, and that person to the next, and so on, and so forth. In case any of you have lost sight of this. This is how an epidemic, and pandemic works. It’s how we got here in the first place. It’s not just about what one person does, or one small group of tipsy teenagers throwing back shots at a crooked table outside a dive bar. It still is about all of us. Its still the same. The virus is still here in plain sight. And there’s still no cure for it.
Let’s all just say for the millionth time. It sucks. It sucks thinking about this all the time. But, we still have to think about it. We still have to think twice before we decide to act like we used to act.. So let’s do that. Think twice.
>MB
Reprinted from Yale School of Public Health: Link>
“Risk of Resurgence” in COVID-19 Epidemic if Connecticut Reopens Too Quickly, YSPH Report Finds
As Connecticut tentatively reopens this week after a two-month shutdown, a new report by the Yale School of Public Health warns that if people resume normal activities and contacts too quickly there will be a “sharp resurgence” in hospitalizations and deaths in the coming months.
Associate Professor Forrest Crawford and postdocs Olga Morozova and Zehang (Richard) Li created a mathematical model to predict COVID-19 transmission, hospitalization and deaths in the state under “slow” and “fast” reopening scenarios.
If the state reopens too quickly, a second wave may be unleashed, the effects of which could be worse than what has already happened. It could result in an estimated total of over 8,100 deaths by September 1 in Connecticut. More than 3,500 state residents have already died from coronavirus.
“If contact rates return quickly to levels seen in early March, the number of new cases could rise dramatically over the summer” said Crawford, the report’s lead author. “Connecticut decision-makers need to closely monitor data on new cases and hospitalizations, as well as transmission model projections, in order to reopen the state safely.”
Under a slow reopening scenario (defined as relaxing restrictions so that contact increases at a rate of 10 percent each month) the incidence of the disease will still increase slightly in the coming weeks but will taper off and stay at lower levels. Hospitalizations for the disease will continue to decline, rising slightly in August and the number of coronavirus-related deaths will rise slowly, with an estimated total of 4,600 to 7,100 by September 1.
Under the fast scenario (defined as increasing contact at a rate of 10 percent every two weeks), Crawford and colleagues found that the number of new infections is likely to spike throughout the summer, potentially exceeding hospitalization capacity and resulting in anywhere from 5,400 to 13,400 total deaths by September 1.
“These projections are based on the latest available data and knowledge from the scientific community,” said Li. “As we gather new evidence about transmissibility of the disease and effectiveness of interventions, our model projections will improve.”
If contact rates return quickly to levels seen in early March, the number of new cases could rise dramatically over the summer.
The researchers attributed the recent decline in hospitalizations to the reduction in contacts following distancing measures implemented by the state officials. “It is too early to return to normal. As some businesses reopen, it is even more important for people to continue practicing social distancing and avoid traveling to highly affected areas, most importantly New York City,” said Morozova.
Yale School of Public Health Professor Albert Ko co-chaired Gov. Ned Lamont’s ReOpen Connecticut Advisory Group, which strongly advised a cautious and conservative schedule as the state starts to return to normal.
“These model projections of the future risk of COVID-19 resurgence directly informed the recommendations made to mitigate this risk,” Ko said. The advisory group, which recently completed its work, was not involved in the preparation of the report.
Other key points from the report include:
- Real-time metrics (such as hospitalizations, case counts and deaths) may not provide adequate warning to avoid a resurgence.
- Closure of schools and the state’s stay-at-home order greatly reduced transmission of the virus.
- There are substantial gaps in knowledge about critical aspects of the disease, including the proportion of infected individuals who are asymptomatic, infectiousness of children, the effects of testing and contact tracing on isolation of infected individuals and how contact patterns may change following reopening.
Reprinted from Yale School of Public Health: Link>
Access full report: Link>
by Michael Bailey | May 22, 2020 | Health & Medicine, Society and Culture |
As I’ve written previously, the decision on how we as individuals react to official reopening announcements should be taken in a serious context first, and foremost, within actual virus transmission rates, and testing volume, and ongoing testing access. I’ve said it before. I will say it again. This virus is still a significant threat to public health, with virtually all the same risk factors that were there from the beginning. What’s changing now is not the virus risk, but the way specific businesses are going to operate within the risk environment. Whether you as an individual feel safe enough with those changes to re-enter these environments, just because there is a legal allowance of sorts, is a question you’ll have to answer in your private deliberation. Don’t expect it to be easy. Personally, I’m with the 72%. -MB
The Country Is Reopening—Now What?
Yale Medicine expert answers commonly asked COVID-19 questions as states begin to reopen.

For many, news that the country is reopening during the COVID-19 pandemic is met with a sense of anxiety and confusion.
Reprinted from Yale Medicine
By Joseph Piccirillo, May 20, 2020
Summer is coming. Usually, the season comes with thoughts of beach days, ice cream, baseball, and day camp. But for many, the prospect of summer during the COVID-19 pandemic is met with an overall sense of anxiety and confusion—and questions.
Is the beach safe? The ice cream shop is open, but should I really go? And more importantly, how are we any better off, in terms of infection prevention and treatment, than we were in mid-March, when stay-at-home orders were first put into place?
In other words, why are we reopening now, and how do we make sense of it all?
“I think it is hard for all of us to wrap our heads around reopening,” says Jaimie Meyer, MD, MS, a Yale Medicine infectious disease specialist. “There is nothing magically ‘safe’ about May 20, and very little difference in epidemiologic risk between May 19 and May 21. Only a public health approach that is data-driven will dictate a slow and measured reopening.”
Reopening criteria confusion
Part of the confusion may lie in the number and scope of documents detailing the suggested criteria required for reopening the country. The White House has a protocol called “Opening Up America Again,” the Centers for Disease Control and Prevention (CDC) has its own version, in addition to six one-page infographics, and some states, including Connecticut, have their own plans, some of which are more or less stringent than the White House’s protocol.
The idea, in theory, is that once the state-specific version of the reopening criteria has been met, it will be safe to begin what’s called a “phased reopening”—in other words, a gradual relaxing of some restrictions, as well as the opening of some businesses. With a phased reopening, state officials (working with county and local officials) are presumably able to monitor the number of COVID-19 cases, and can move forward with—or stop, if need be—further reopenings, or phases, based on changes in those case numbers.
But many states have opted to overlook federal criteria—or create their own smaller-scale benchmarks—and move forward with a phased reopening anyway, leaving it up to individuals to make their own decisions about when and how to venture outside safely.
Most Americans are worried about this. According to a recent Reuters national poll, 72% of adults in the United States said people should stay at home “until the doctors and public health officials say it is safe.”
With that in mind, we spoke with Dr. Meyer, who provided answers to frequently asked questions about COVID-19, especially as it relates to the reopening of the country.
The interview has been edited for length and clarity.
Q. Why is it important to have a consensus on the criteria for reopening?
A. The purpose of having standards for a phased reopening is to ensure that the response is data-driven. I strongly believe that if criteria are not met, we risk an uptick in new cases and a setback in terms of progress with this disease.
Q. What does a data-driven public health approach to reopening look like?
A. Five things, really. 1) The presence of protective immunity. There are a number of people (depending on where you live) who have now been infected with SARS-CoV-2, recovered, and have potentially developed antibodies against the virus. Although it’s not clear yet whether these antibodies will completely protect them from reinfection, at what level and for how long, there is likely some protective immunity; 2) The ability for hospitals to care for patients. As hospitals reduce their overload, they will have expanded capacity to care for people who become sick; 3) Adequate testing. Testing is expanding (or should be) in most states, increasing the potential to identify people who are sick and isolate them; 4) Contact tracing. This is also scaling up (or should be) in most states, increasing the potential to identify even more people who are infected and isolate them; and 5) Careful restrictions on social distancing, cleaning and disinfecting, and PPE [personal protective equipment] in public spaces, all of which reduce the spread of disease.
We need all of these components together to keep the curve going down and to prevent a second wave.
Q. Before a safe and effective vaccine is developed, is the goal to make the virus disappear or to let people get infected, but at slower rates that hospitals can keep pace with?
A. The goal of the combined public health measures I just mentioned is to reduce the number of new cases which, in turn, reduces the number of hospitalizations and the number of COVID-related deaths. No one can expect that these measures will “disappear” the virus, or that everyone will eventually become infected. The truth will likely lie somewhere in between, but only the data will tell us exactly where.
Q. How can we be sure that testing is accurate across all states?
A. It’s hard to know. There are a wide variety of types of tests being used across health systems, and they have varying degrees of sensitivity—meaning the ability to pick up ‘true positives’ for people who actually have the disease—and specificity, which is the ability to tease out ‘true negatives’ for those who do not have the disease.
Tests generally fall into three major categories: tests that look for the genetic material [RNA] of the virus; “antigen” tests that look for a particular part of the virus; and “antibody” tests that look for the human body’s response to the virus.
Some of these tests have been fully vetted and validated before they were approved by the FDA [Food and Drug Administration], and others were authorized under an emergency use authorization [EUA] but have not yet been fully vetted and validated. We are really learning on the fly.
Q. Why is there still a delay in the number of tests being made available?
A. This relates to the capacity to collect the samples, availability of materials to run the tests (nasal swabs or liquid reagents to process the samples, for example), and certified labs to analyze the tests.
Q. The FDA issued two EUAs for at-home tests, one for a nasal swab sample and, more recently, one for a saliva sample. Does that mean we will be able to pick these up at a drug store for routine testing?
A. Yes, home collection kits are likely headed our way. This is exciting because it will not only make the tests more widely available, but also reduce risks of exposure to health care workers that can happen during the collection process. But, I believe home collection kits will still need to be ordered by a health care provider instead of being available over the counter.
Q. What is contact tracing? If I am contacted, does that mean I have the virus?
A. Contact tracing is a way to identify those who have been exposed to people with confirmed cases of COVID so they can get tested—it’s a key component of disease containment strategies. Departments of Public Health everywhere, including in Connecticut, are ramping up their ability to conduct contact tracing. They already have systems in place for other highly communicable diseases, such as syphilis, so I imagine it will operate in a similar way.
If you are contacted, it means you had a potentially high-risk exposure to someone who was infected with COVID. This is not a reason to panic, but rather a reason to self-isolate and get tested.
Q. For how long will we have to wear masks?
A. We may have to have some sort of barrier protection for our faces, like cloth face coverings, until we have highly effective vaccines available.
Q. So, it could be for a while—years, even.
A. Yes.
Q. How does wearing a surgical mask or a cloth mask protect others if small particles carrying the virus can still get through?
A. I like to think of facial coverings as putting your thumb over a hose—some water may escape, but the major flow is blocked. Facial coverings like cloth masks prevent many particles from being disseminated into the environment, but not all. That is why we need social distancing and other prevention strategies, like hand washing and cleaning or disinfection, in addition to cloth masks.
Q. The six-foot physical distance is based on previous coronaviruses, correct? Is it enough? If I am around runners or people who are coughing a lot, should I move farther away?
A. Yes, that’s true. If people are coughing, sneezing, or breathing heavily they may aerosolize more droplets, which may be propelled further. That is why we ask people who are sick to stay home, wear facial coverings, and remain socially distant.
Q. If you’re running for a long distance behind someone, though, wouldn’t that increase your risk? Is it better to move across the street?
A. There is no data on whether it is better to run behind, in front of, or to the side of someone while running. The best bet is to run at least six feet apart, regardless of the direction.
Q. There was a study in The New England Journal of Medicine (NEJM) about SARS-CoV-2 being in aerosols and remaining in the air for three hours. Is that the same as airborne transmission?
A. This means that once virus-coated droplets are sprayed into the air, they can remain there and survive for up to three hours. This facilitates airborne transmission of the virus from person to person, because that live virus can infect someone else if it enters their respiratory tract.
Q. Wouldn’t that mean that we are all susceptible to potential infection in any enclosed space, even if we all wear cloth face coverings?
A. We have to be careful when we translate lab experiments into real-life scenarios. The experiment discussed above found that live virus could be recovered from aerosol for up to three hours, but it’s not known whether the quantity is enough to actually cause infection in someone else.
As the state/country reopens, however, we know that better-ventilated spaces result in less distribution of the virus-laden droplets. This is the reason for states recommending reopening of outdoor spaces first, where transmission is less likely, especially with social distancing.
Q. That means that two families who are on separate blankets six feet apart at the beach would be relatively safe, even if they stayed on their blankets for 8 hours or so, breathing in the same air.
A. Yes.
Q. Some people think they’ve already had COVID-19 in December or January. Is there a way for people to know if they had it? And if they did, do they have some immunity?
A. People who have COVID-19 (whether or not they were ever officially diagnosed) and recover often develop antibodies against the virus. Antibody tests have been developed but are problematic because of high rates of false negatives and false positives. So, right now it’s not recommended that they be used to make individual decisions about personal health or safety. We suspect that antibodies will offer some protection from reinfection, but it’s not known what level of antibodies is sufficient and how long that protection will last.
So, we don’t want people going out to get tested for antibodies and then feeling falsely assured that they are protected.
Q. When returning from the grocery store, is it really a smart strategy to wipe down packaged food with bleach wipes, or is it overkill? If a delivery driver with COVID sneezed on or near my cardboard Amazon package and then dropped it off on my doorstep and I picked it up immediately and opened the box, could I get sick?
A. I think we need to balance anxiety with practicality and safety. I suggest that people practice reasonable precautions. This means unpacking groceries/deliveries from their containers or boxes, washing hands, and wiping down countertops with bleach. Even though the virus can be found on cardboard for up to 72 hours, the NEJM article suggests viable [live] virus is probably on cardboard for closer to 8 hours. Your best bet is to wash your hands after handling potentially contaminated surfaces.
Q. Do we know how long someone is contagious when they’re asymptomatic?
A. People can shed virus (and potentially infect others) for three to five days prior to developing symptoms. Those who don’t develop symptoms at all can shed virus for approximately 14 days at high enough levels that they may be contagious to others.
People can shed virus for weeks following recovery, but we think that this is either dead virus or virus at low enough levels that they are not contagious to others.
Q. In Connecticut, gatherings of 5 or fewer are OK, and most people have been sheltering-in-place for about two months. So, is it safe for one person to have an indoor visit with someone else if both have sheltered-in-placed for two months and have not had any symptoms for 14 days?
A. Data from over 1,000 people hospitalized in a single week in New York showed that the majority of people infected and newly admitted were people who identified as “mostly staying home.” The likely reason for this discrepancy was that there were gaps in home isolation behaviors—social visits with others, being in public spaces without face coverings or appropriate hand hygiene, interacting with others without taking precautions, etc. I know many people who would say they are fully isolated, but are still spending time in public spaces. So, if both people were truly isolated, it would be reasonable to have a visit without any additional risk. Ideally, people could get tested before they gather together.
Q. Some have missed a mammogram or a colonoscopy or a dental procedure, and they’re afraid to go to the doctor. Is there a safe way to get these things done?
A. Over the next few months at Yale New Haven Hospital, we are looking towards reopening ambulatory services and elective procedures, as are places elsewhere that are on the downside of their COVID curve. I think telehealth will be with us for the foreseeable future at least to some extent. In the earliest phases of reopening, in-person care will likely be prioritized for urgent health concerns. But please don’t miss your routine vaccines and health screenings as we move forward in reopening. General preventive healthcare remains important for long-term and overall health.
Q. What do you think needs to happen before you’re confident that we can get this under control?
A. Expanded testing and contact tracing. Safe and effective vaccines. Effective treatment. All are on the horizon and scientists globally are working at a breakneck pace to make these a reality.
Q. Anything you want people to know as we start to reopen around the country?
A. People who have underlying health conditions that place them at higher risk of severe COVID-19 will need to practice precautions for the foreseeable future. I know everyone has COVID fatigue. We have message burnout, are tired of being home, and mourn our “regular” lives. But reopening must be paced and careful and responsive to data so that we don’t backtrack.
Unsure about a COVID-related term? Click here to read Yale’s COVID-19 glossary.
Learn more about Yale’s research efforts and response to COVID-19.

by Michael Bailey | May 20, 2020 | Economics, Health & Medicine, World Events |
I’d like to believe most people don’t need to read articles like this one in order to understand common sense and perspective. I’d like to.
What’s about to happen this week is based in gigantic proportion on economics. That’s a super valid concern. It deserves some kind of response. But, it should NOT be a significant signal about the reduction of public heath risk to widespread Covid infection.
A reasonable, common sense approach to understanding what the risk reality is right now in this country lies not in solely listening to commercially funded TV or radio news programs, most politicians, vociferous family members, friends, or even, business owners.
The intelligent and rational way to decide when, where, how, and why all of us re-open our own lives, is by reading and understanding transmission rates through public health sources, publicly funded news outlets, respected epidemiologists, science and medical professionals, closely studying and following the arc so far.
We all want to return to normalcy, but this crack of daylight in the wall of sequestering, should not be mistaken for any meaningful symbol of all clear. Not by a long shot. NOT by a long shot.
If you’re on the fence, get off it by reading and sourcing good info, data and opinions, as far away as possible from vested interests, or anyone who has a bone to pick for/against political entities. Let knowledge and fact be your guide, not pressure by friends, family, retailers, politicians, or a weakness of will.
This is a public health issue. It is your health issue. It is my health issue. This is the priority for where it should begin and end.
MB
Article below reprinted from Business Insider
How to decide if it’s worth the risk to return to malls, gyms, salons, and more as states reopen but experts remain cautious.

AP Photo/David J. Phillip
-
Shops, restaurants, salons, gyms, and even bowling alleys are opening across the US as states loosen their shelter in place orders.
-
Experts say it is important to realize that returning to businesses can still be risky, and answers on safety are far from black and white.
-
You can determine risk by weighing factors such as if you can stay six feet away from others, if everyone is wearing masks, and what the prevalence of the coronavirus is in your area.
-
Different types of businesses come with different risks, meaning that concerns about returning to restaurants, stores, salons, and gyms need to be examined separately and together.
As businesses reopen across America, many people are confused about what exactly is safe and what isn’t.
Experts say that just because restaurants, stores, and even nail salons are open, does not mean that they are necessarily safe to visit. Instead, it means that people have the ability to choose if they want to take the risk of returning.
“The one thing we do know is the virus is still out there,” said Dr. Celeste Monforton, a lecturer in public health at Texas State University. “When some governor said, May 1, we’re opening things up — It’s not like the virus had a calendar and said, okay, I’m going underground again.”
Monforton and Dr. Jaimie Meyer, an assistant professor of medicine at Yale School of Medicine, told Business Insider that they understand why people are confused, as the CDC, the White House, and state governments have released different and sometimes conflicting guidelines.

AP Photo/LM Otero
Both Meyer and Monforton also understand the economic argument for businesses to reopen. And, neither believes everyone should avoid all businesses, all the time.
“I almost would never say anything in absolute, because I think when you say things like that, people just tune out,” Meyer said. “It’s too hard for people to lose that much control over their lives.”
However, Meyer says people should be aware of COVID-19 cases and the risk of infection in their communities, not simply if it is legal or not for businesses to reopen. While different people have different tolerances for risk, Meyer says she personally is advising family and friends to err on the side of caution.
“There are so many unknowns here,” Meyer said. “Everything that I do, I ask myself, if I got sick from doing this, was it really worth it?”
Certain factors can help determine if a business is safe.

AP Photo/David J. Phillip
As states reopen, these experts say that risks exist on a spectrum.
Meyer and Monforton resisted saying any type of business was definitively more risky than others. For example, a bowling alley where there is constant cleaning and social distancing could actually be safer than a grocery store that hasn’t added any new safety measures since the pandemic.
Instead, there are a few big-picture factors you can use to determine if a business is safer — though not 100% risk-free — to visit.
Questions that can help determine how risky it is to visit a business include:
- Can you stay at least six feet away from other people in the space?
- Is everyone wearing masks? Wearing a mask doesn’t necessarily prevent you from catching the coronavirus — but other people wearing masks reduces the likelihood they will spread it.
- Can you stay outside or minimize your time indoors?
- Are workers regularly cleaning the space?
- Are employees and customers able to wash their hands?
- Have the number of COVID-19 cases in your community decreased over the last two weeks?
- Is there limited community spread of the coronavirus in your area?
If you can answer “yes” to all of these questions, there is less of a risk of catching the coronavirus, whether you are considering visiting a restaurant or a mall.
You can also take steps, such as washing your hands and wearing a mask, to make your community safer even when businesses and governments do not require it.
Waiting a few more weeks to go shopping or get your nails done could also help everyone understand the situation better.

AP Photo/LM Otero
At this point, Meyer is encouraging people to behave as if everyone in public is infected with the coronavirus and act accordingly — maintain six feet of distance, wear a mask, and wash your hands regularly if you’re leaving your house.
“If you don’t practice social distancing and hand washing and wear masks, we’re going to experience a major setback and there will be a second wave,” Meyer said.
Still, planning to stay inside for 18 months is a daunting idea.
Instead, Monforton says that she is encouraging people to take things week by week. Every week, scientists and healthcare professionals find out more about the coronavirus. Even one extra week of knowledge can help customers and business owners make better decisions as states reopen.
“We’re going to learn a lot in the next couple of weeks and that’s going to be continuing to inform people about the risk — whether the risk is higher than we expected when things opened up [or] less than we expected,” Monforton said.
Older people and those with preexisting conditions should take more steps to reduce their risk, avoiding activities that people with a higher tolerance for risk may be willing to participate in. Everyone should understand that when they make a nonessential trip to a store, restaurant, or gym, it might not only impact them — if they haven’t been tested recently, they could unknowingly spread the coronavirus in their community as an asymptomatic carrier.
While no specific type of business is necessarily riskier or safer than others, we already know that each category carries different types of risks.
Here is a breakdown of some of the risks that come with different types of businesses, as well as some ways a risky situation can become safer.
Restaurants can be risky, but there are ways to support your favorite spot without endangering yourself.

AP Photo/Russ Bynum
The good news for restaurants is that experts say even if a worker coughs or sneezes directly in your food, you won’t catch coronavirus from eating the meal.
The bad news is that customers crowding into a restaurant or bar could put everyone at risk of catching the coronavirus. Social distancing can be difficult for workers in kitchens. Many restaurants will not be able to maintain necessary social distancing while also bringing in as many customers as they did pre-coronavirus.
The National Restaurant Association has extensive guidance on how restaurants can reopen relatively safely.
These adjustments could make restaurants safer:
- Serving food via drive-thru, takeout, or delivery.
- Adding more sidewalk and curbside pick-up options.
- Adding outdoor dining.
- Reducing the number of tables.
- Requiring reservations to limit the number of customers.
- Training staff to monitor for symptoms.
Shopping malls and stores will need to limit how many people are allowed in.

AP Photo/LM Otero
Monforton says she expects stores of all types to follow grocers’ blueprints. Even if Macy’s is selling dresses instead of shoes, things like plexiglass barriers, new cleaning routines, and hand sanitizing stations will transfer over.
Malls create different issues, as customers are likely to visit several stores during one trip. This can make it more difficult to limit how many people enter a store, something that is crucial for social distancing.
Ultimately, the biggest differences between essential and nonessential stores is what they’re selling — not the risk levels. Meyer is encouraging friends and family to avoid unnecessary risks, such as shopping for nonessentials. But, retailers are trying to accommodate those willing to take the risk that is associated with any type of shopping trip.
The National Retail Federation has a full guide for what stores should do to reopen.
Here are some changes that stores can make to become safer to visit:
- Limiting how many people are allowed inside to allow for social distancing.
- Promote “contactless” shopping, such as self-checkout and curbside pick up.
- Ban people from testing beauty products, unless they are using single-use testers.
- Stopping services such as alterations and ear piercing.
Risks associated with working out make gyms and fitness centers especially dangerous.

Maranie Staab/Reuters
Meyer said that people should be “especially cautious” at gyms, fitness centers, and other places where people work out as businesses reopen.
“When people are working out and breathing hard, they are more likely to transmit droplets,” which could spread the coronavirus, Meyer said.
This makes cleaning practices and social distancing even more important. So, if you’re willing to take the risk of returning to work out, make sure you can stay at least six feet away from other people and that the business has a strict cleaning schedule in place.
How fitness studios and gyms can make things safer:
- Offer virtual classes, instead of having people attend classes in person.
- Limiting the size of classes or providing one-on-one classes.
- Offering outdoor workouts.
- Taking people’s temperatures and making sure they don’t have symptoms before entering a studio or gym.
- Having people bring their own equipment, such as yoga mats and weights.
- Requiring people to wear masks while working out.
Salons and barbershops make it difficult to social distance.

Associated Press
One of the biggest risks associated with barbershops, as well as hair and nail salons, is that the nature of the activity makes it impossible to keep six feet in between people.
“If you’re one of these high-risk individuals … it’s probably not safe yet,” even with changes, Meyer said.
The American Industrial Hygiene Association acknowledged that nail and hair salons have been “very challenged” during the pandemic in their guidelines for reopening.
A few ways salons and barbershops can make things safer:
- Disinfecting between visitors.
- Limiting how many people are inside the salon or shop at one time.
- Employees and customers should wear masks and gloves.
- Closing the reception area and having people wait outside until it is time for their appointment.
Bowling alleys, arcades, and other interactive indoor spaces are extremely risky.

AP Photo/Paul Newberry
Georgia’s decision to allow bowling alleys to reopen raised some eyebrows.
“Entertainment is important and, for many people, perhaps bowling alleys are very important entertainment,” Meyer said.
However, Meyer continued, the problem with bowling alleys, arcades, and similar businesses is that they are closed in and high-touch.
In a bowling alley, you are going to be in an enclosed space with other people for a significant period of time, which is risky in and of itself. Additionally, you are touching things that a lot of other people are touching. It is basically impossible to sanitize items like bowling balls every time they touch people’s hands or other potentially contaminated spaces.
At this point in time, places like bowling alleys — as well as anywhere with crowds of people — are high on the list of places to stay away from if you want to avoid catching COVID-19.
Bowling alleys are never going to be the safest choice. Here is how they can be safer:
- Constant sanitation.
- Making people bring their own balls.
- Having people wear masks.
- Requiring people to stay six feet away from each other.
Business Insider, Kate Taylor, May. 15, 2020, 07:24 PM